By Daniel Fontaine
The recent release of the Office of the Seniors Advocate’s (OSA) Quick Facts Directory, along with the subsequent media attention, has highlighted a number of challenges facing residential care homes in British Columbia, focusing on the need for increased staffing levels for seniors in residential care.[i]
As a result of the OSA report, the BC Ministry of Health announced in early April 2016 that it will be undertaking a review of staffing guidelines in government-funded long-term care homes for seniors. In particular, BC Heath Minister Terry Lake requested the Ministry undertake a review to examine how health authorities are funding seniors’ homes, including looking at the care hours being provided to seniors, especially those living with dementia and other ailments. [ii] Further details on this review are still forthcoming, and the BCCPA, which in general supports such a review, looks forward to discussing the care hours being provided to seniors with the Ministry of Health, as well as on the development of any new strategies to deal with health human resource issues more generally.
As a starting point for these discussions, the BCCPA would like to provide further insight into the complex issues that exist regarding Direct Care Hours in residential care homes. Direct care hours (DCH) are the time that healthcare professionals, including Registered Nurses, Licensed Practical Nurses, Physio- and Occupational Therapists, Residential Care Aides and others, dedicate to caring for their residents each day. DCH do not include hospitality services such as meals, laundry or housekeeping.
According to a 2015 Insights West survey of over 800 British Columbians commissioned by the BCCPA, 78% of respondents believe regardless of where you live, the number of DCH funded by Health Authorities for a senior with similar levels of acuity should be the same. In reality, however, significant disparities exist in BC with respect to DCH among care homes within and between Health Authorities. For example, an https://bccare.ca/wp-content/uploads/2022/08/medcare-img22.jpgistrative report from Vancouver Island Health Authority shows differences of DCH among care homes between 2.81 to 4.98 with a median of 3.18.[iii]
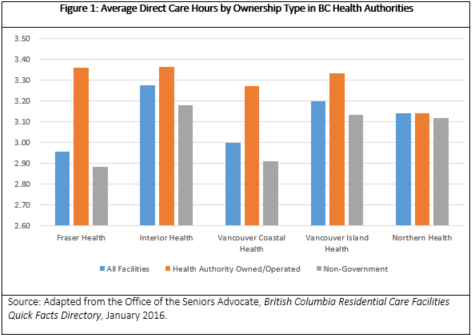
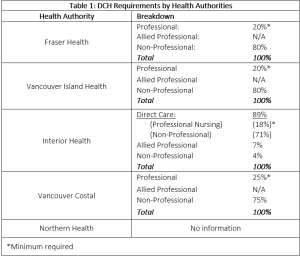
Differences in DCH are also outlined in the Quick Facts Directory recently published by the OSA, which demonstrates discrepancies both by health authority region, as well as ownership type (see figure 1 and 2).[iv] Table 1 below outlines further differences in DCH requirements by the various Health Authorities including with respect to the breakdown of staffing. With such disparities it makes it difficult to provide equal and consistent levels of care, leaving some seniors at a disadvantage over others.
In BC, like most provinces, there are no specific provincial requirements for a number of DCH that must be provided on average to each resident per day. Likewise, there are no specific requirements for the type or mix of staff that must be on duty. Instead, there are, however, some outcome-based staffing standards, which are contained in the Community Care and Assisted Living Act (CCALA) and accompanying residential care regulations.[v]
In 2009, the BC Ministry of Health provided health authorities with a framework to assist in the development of their three-year plans. The health authorities used cost assumptions provided by the framework to ensure plans reflected a consistent provincial approach to residential care staffing. In particular, one of the cost assumptions was that there would be 3.36 hours of direct care provided per day per resident (3.00 hours nursing and 0.36 allied, or supporting care).[vi] The Ministry, however, has indicated clearly that this number of DCH was to serve only as a guide for health authorities.[vii]
In the 2012 Ombudsperson report on seniors care, it also recommended the BC Ministry of Health establish appropriate staffing mixes including a minimum number of DCH and number of staff required at different times in residential care homes. Likewise, the report recommended the Ministry work with health authorities to conduct an evaluation to determine whether residential care budget in each health authority is sufficient to meet the current needs of its population; and establish consistent method to determine funding requirements of residential care homes.[viii] The same report also notes that the costs of moving to the 3.36 can be quite significant.
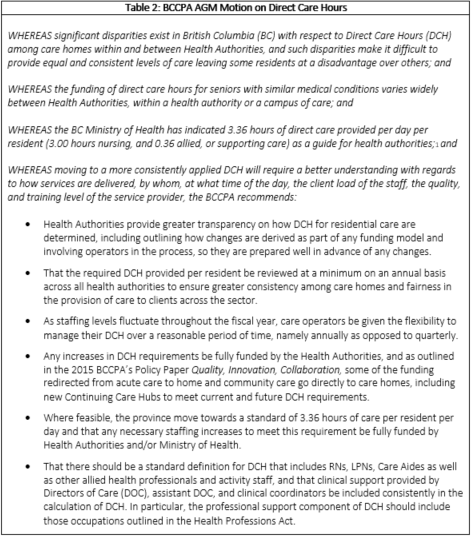
While the BCCPA supports moving towards a 3.36 DCH, or another appropriate standard based on best practice, any move to this to meet such a requirement should be fully funded by Health Authorities and/or the Ministry of Health.[ix] These and other tenets are outlined in the motions that the BCCPA will be putting forward at its 2016 AGM as part of its Annual Conference (see table 2).[x] As outlined, one the recommendations in the motion is that “where feasible, BC move towards a standard of 3.36 hours of care per resident per day and that any necessary staffing increases to meet this requirement be fully funded by Health Authorities and/or Ministry of Health.”
Likewise, as recommended in 2015 BCCPA report entitled Quality, Innovation, Collaboration: Strengthening Seniors Care Delivery in BC it advocates that Health Authorities redirect a minimum of 1% annually over a five-year period to the home and community care sector. The BCCPA believes not only could this help deal with existing cost pressures facing service providers it could help support development of new care models, particularly new Continuing Care Hubs in order to better meet current and future DCH requirements. [xi]
The BCCPA hopes that the government review on DCH and funding that will be undertaken can address many of the concerns that have been expressed by care providers and in the media. In particular, this includes ensuring that non-government care operators can remain financially viable while also providing seniors with high quality care.
Click here for additional resources.
END NOTES
[i] BC Office of the Seniors Advocate. Residential Care Facilities: Quick Facts Directory. January 2016. http://www.seniorsadvocatebc.ca/wp-content/uploads/sites/4/2016/03/BC-Residential-Care-Quick-Facts-Directory-2016.pdf.
[ii] Vancouver Sun. BC Health Minister Orders Review of Staffing Guidelines in Long-Term Care Homes for Seniors. April 7, 2016. http://vancouversun.com/news/local-news/b-c-health-minister-orders-review-of-staffing-guidelines-in-long-term-care-homes-for-seniors
[iii] Administrative Report for Residential Care Facilities 2014 Quarter 3 (Oct – Dec 2014) Vancouver Island Health Authority.
[iv] BC Office of the Seniors Advocate. Residential Care Facilities: Quick Facts Directory. January 2016. http://www.seniorsadvocatebc.ca/wp-content/uploads/sites/4/2016/03/BC-Residential-Care-Quick-Facts-Directory-2016.pdf. According to data outlined in this report of the 292 government-funded facilities, 232 did not meet the ministry’s staffing guideline, a recommendation of 3.36 hours of care per senior every day.
[v] As outlined in Section 42 (1) of the Residential Care Regulations: A licensee must ensure that, at all times, the employees on duty are sufficient in numbers, training and experience, and organized in an appropriate staffing pattern, to (a) meet the needs of the persons in care, and (b) assist persons in care with activities of daily living, including eating, mobility, dressing, grooming, bathing and personal hygiene, in a manner consistent with the health, safety and dignity of persons in care. To access Residential Care Regulations, click here: http://www.canlii.org/en/bc/laws/regu/bc-reg-96-2009/latest/bc-reg-96-2009.html#history
[vi] Home and Community Care Program, “Costing Assumptions #3 for the Proposed Staffing Framework for Residential Care Facilities,” 11 August 2009, 1.
[vii] Home and Community Care Program, “Residential Care Staffing and Reporting Tool Frequently Asked Questions,” internal document, 3.
[viii] Ombudsperson. The Best of Care: Getting It Right for Seniors in British Columbia. Part 2. February 2012. Accessed at https://www.bcombudsperson.ca/seniors/seniors-care-investigation/seniors-report-part-two. In research and consultations conducted by the Ombudsperson they found that the recommended range of care hours was generally between 3.2 and 4.0 hours per resident per day.
[ix] In 2009, the BCCPA had previously recommended adopting 3.2 hours of care per resident per day as the preferred provincial standard for residential care homes, and 2.8 hours as the baseline standard. It also recommended that all residents be assessed using tools currently used in health authorities to determine the actual direct care hours of each resident and, therefore, the total required hours in a care home. Source: Residential Care Health and Safety Guidelines. Spring 2009. BC Care Providers Association. Accessed at: https://bccare.ca/file/bccare_safety_grid_v11.pdf
[x] BCCPA. Three Special Resolutions Will Be Debated at 2016 AGM. April 1, 2016. Accessed at: https://bccare.ca/bccpa-members-to/
[xi] BCCPA. Quality-Innovation-Collaboration: Strengthening Seniors Care Delivery in BC. September 2015. Accessed at: https://bccare.ca/wp-content/uploads/BCCPA-White-Paper-QuIC-FINAL-2015.pdf.