COVID-19 and its effect on seniors care
Most jurisdictions across the world have been affected in some way by the COVID-19 pandemic. Along with workers, particularly hard hit have been seniors – including those living in long term care where many are already increasingly frail and suffering from multiple chronic conditions.[i]
To protect vulnerable populations, jurisdictions in Canada (including BC) and internationally have taken various approaches to prevent and reduce the spread of COVID-19, such as the increased use of personal protective equipment (PPE), implementing infection prevention and control (IPC) measures and by limiting those who can visit or work at seniors care homes. Despite these actions, the long-term care sector in Canada has been particularly hard hit, accounting for the majority of COVID-19 related fatalities.
 In late June, for example, the Canadian Institute for Health Information (CIHI) issued a report highlighting that long term care residents made up 80 per cent of all reported COVID-19 fatalities in Canada, in contrast to an average of 42 per cent among other countries studied.[ii] These findings were reiterated in an October 2020 report by Public Health Agency of Canada (PHAC) noting that as of mid-August, Canada had one of the highest fatality rates among long term care residents out of the 37 countries in the OECD.[iii] A recent study analyzing deaths per 100 population, however, shows Canada in the middle of countries surveyed when looking at number of residents per 100 living in long term care (see Figure 1).[iv]
In late June, for example, the Canadian Institute for Health Information (CIHI) issued a report highlighting that long term care residents made up 80 per cent of all reported COVID-19 fatalities in Canada, in contrast to an average of 42 per cent among other countries studied.[ii] These findings were reiterated in an October 2020 report by Public Health Agency of Canada (PHAC) noting that as of mid-August, Canada had one of the highest fatality rates among long term care residents out of the 37 countries in the OECD.[iii] A recent study analyzing deaths per 100 population, however, shows Canada in the middle of countries surveyed when looking at number of residents per 100 living in long term care (see Figure 1).[iv]
COVID-19: Seniors Care and Living in BC
While British Columbia has fared better than other provinces in terms of the number and percentage of deaths in long term care (see Figure 2) the effects of COVID-19 have still been devastating to providers, seniors and their families.[v] In response to COVID-19 there have been numerous actions and steps taken provincially to protect seniors although some have questioned whether these directives, along with efforts to test residents and staff for COVID-19, were applied quickly or comprehensively enough.[vi]
While in BC there was a decline in number of COVID-19 long term care outbreaks over the summer reaching close to zero, the province has seen increases over time (see Figures 3 and 4) particularly as community transmission increases as this is one of the main contributing factors for such outbreaks.[vii] As of mid-October, for example, BC had 17 long term care and assisted living sites with COVID-19 outbreaks, while the number in Ontario (86) had also quadrupled over the past month, and other provinces such as Quebec (39), Manitoba (7) and Alberta (13) [viii] were also dealing with outbreaks coinciding with overall increases in the community.[ix]
Less than a month later BC, as of mid-November, BC reached its highest level of current outbreaks with over 40 long term care or assisted living sites in outbreak status. While younger age groups have largely been driving infections during the second wave, the cases are now starting to enter seniors care homes.[x]
Navigating the Next Wave
As cases continue to increase and as jurisdictions enter the second or even third waves of the pandemic, BC Care Providers Association (BCCPA) believed it was important to be better prepared. Therefore, in late July, the BCCPA’s Advisory Committee on COVID-19, issued initial draft recommendations to better prepare government and the sector.[xi] In total, 17 initial recommendations were issued under four key areas or themes including: 1) Pandemic Preparedness & Coordination; 2) Reduce Infection Transmission; 3) Support Staff and Operators; and 4) Provide Social Supports.
BCCPA thought it was also important to engage with care providers and other stakeholders to discuss these recommendations further and also identify any further areas or gaps not initially outlined. In coordination with BCCPA, this engagement process was led by the Howegroup and also included a comprehensive survey and literature review. Based on findings from the engagement process, BCCPA has released its final report titled Review of The Response To COVID-19 In Seniors Care and Living which, as discussed later on, will also be the focus of the next Care to Chat event.
Highlights of report including Literature Review
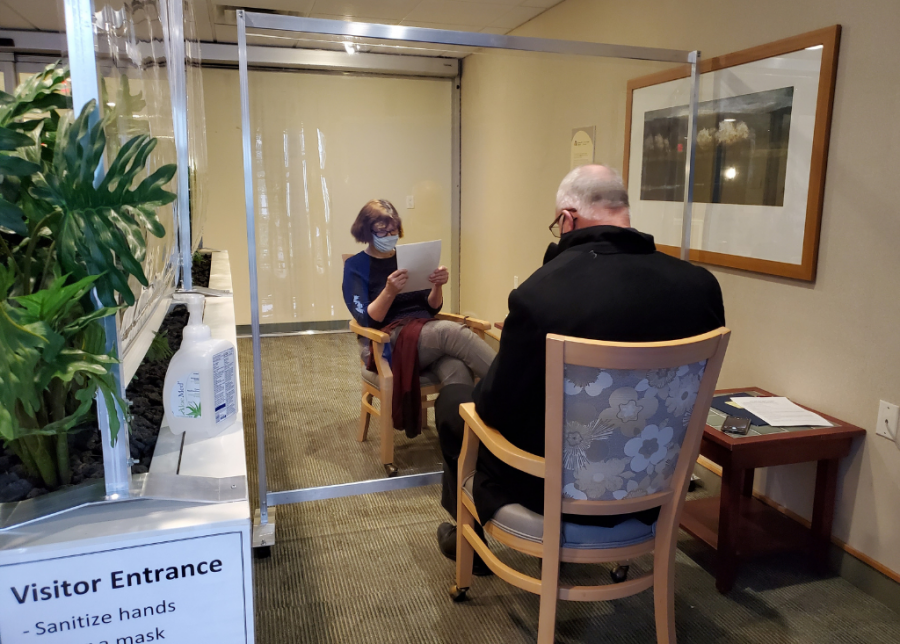
As outlined in the latest report, it provides 24 recommendations under the four key areas outlined earlier such as developing appropriate plans and communication processes; reducing transmission through greater use of PPE, testing and IPC measures; addressing staffing and training issues; as well as providing social supports including improving quality and ensuring safer family visits for seniors.
Along with discussing actions that helped flattened the overall curve and factors that have contributed to transmission, the final report discusses other areas or challenges such as the many health human resources (HHR) challenges (i.e. single site order, wage leveling and pandemic pay), PPE shortages, inconsistent communications, having designated COVID-19 units, financial impacts to providers as well as ensuring senior and working rights. These were also identified in the literature review which also helped assist with the development of report including highlighting the following areas:
- What other countries have done with respect to COVID-19 in seniors care;
- Various issues such as community transmission, focus on acute care, etc.
- What Canada and other provinces have done to deal with COVID-19 in seniors care;
- What BC has done with respect to COVID-19 in seniors care; and
- Outline any potential gaps or other recommendations.
As outlined in the literature and seen by experiences in other jurisdictions the initial recommendations were well supported. For example, the need for proper and regular inspection processes is critical. The single site order has also been effective including one U.S. study showing significant decreases in transmission and possibly reducing death rate in long term care by almost 45 percent.[xii] This, however, will need to be supported by addressing issues such as wage levelling but also ensuring that the single site orders do not exacerbate existing shortages. The use of designated COVID-19 units has also been effective and is used in various jurisdictions world-wide. The literature review also shows how having multi-bed units can facilitate the spread of COVID-19 within care homes as seen in Ontario and other jurisdictions (i.e. Nova Scotia’s Northwood). Having access to appropriate PPE, including proper training and funding are also critical as is providing social supports for families and residents.
While the literature review supports the recommendations there were a few areas or gaps that were outlined that had not been reflected in the initial recommendations but have now been incorporated to some degree in the final report, including:
- Greater focus on developing a testing strategy for workers and residents;
- Better ensuring quality of care and quality of life for seniors;
- Designated Infection Prevention and Control (IPC) staff resources and training; and
- Supports for community care (including home care).
Some additional areas as outlined in the literature review that may warrant further consideration as we move forward also include:
- Supporting changes to physical environment in long term care environments beyond just reducing multi-bed rooms such as physical redesign changes, new models of care (i.e. household care model);
- Supporting innovation, including use of technologies; and
- Increasing surge capacity for care homes or facilities that are in dire need, including formalized support teams.
As outlined earlier in the literature review, for example, the physical environment of a care facility has a critically important role in infection prevention and control. In particular, there are potential advantages of self-contained small homes (e.g., 12-16 bed households) with clustered arrangement of rooms, activity and dining areas — for more effective IPC, responsive management of residents with dementia and care interactions. Smaller group size also provides the option to better compartmentalize residents who might be at greater risk of infection, as well as isolate residents who are infected.[xiii]
Community Transmission
As outlined earlier, one the main factors for COVID-19 outbreaks in long term care or assisted living is also having high levels of community transmission. An October 2020 report by the American Health Care Association/National Center for Assisted Living, for example, shows that cases in nursing homes correlate directly to community spread.[xiv] Another recent study also highlights that where nursing home staff live is a large and significant predictor of which facilities will experience a COVID-19 outbreak.[xv] Overall, this makes sense as with larger levels of COVID-19 in the community, staff who work in care homes are also more likely to get infected and, hence, unknowingly bring the virus into seniors care homes.
How we will prevent greater levels of community transmissions from entering long term care or assisted living will involve not only taking direct measures at the care site such as enhanced screening precautions, increased use of PPE and IPC measures it should also include more aggressive steps such as greater staff testing. An August 2020 research study from the US, for example, concluded that weekly testing of at least half of staff members and residents was necessary to minimize outbreaks in long term care.[xvi] It is also why the BCCPA is putting forward the development of a testing strategy for seniors care and living at its upcoming AGM.
Likewise, other areas to reducing the effects of community transmission among workers is through public awareness campaigns to ensure staff must keep their personal “bubbles” small, avoid attending large gatherings and do not come into work when feeling any symptoms of illness. Likewise, it could also include advocating for stronger public health measures to reduce community transmission such as mask mandates or even stay at home orders.
Care to Chat
 Overall, the final report should serve as a guide as we move forward to better protect most vulnerable populations, particularly seniors. It will also be focus of next Care to Chat event titled COVID-19 and Seniors Care in BC: Navigating the Next Wave to be held virtually via Zoom on Friday, November 27th. In particular, building off these findings and discussions at the BCCPA Virtual Conference in September, this Care to Chat will also highlight how we can better prepare and mitigate the effects of COVID-19 in seniors care and living in the four key areas or themes outlined earlier.
Overall, the final report should serve as a guide as we move forward to better protect most vulnerable populations, particularly seniors. It will also be focus of next Care to Chat event titled COVID-19 and Seniors Care in BC: Navigating the Next Wave to be held virtually via Zoom on Friday, November 27th. In particular, building off these findings and discussions at the BCCPA Virtual Conference in September, this Care to Chat will also highlight how we can better prepare and mitigate the effects of COVID-19 in seniors care and living in the four key areas or themes outlined earlier.
A panel moderated by BCCPA CEO Terry Lake, and consisting of experts including providers from the BCCPA COVID-19 Advisory Committee as well as academia who also assisted with the review will discuss these and other important issues. Along with the formal panel discussion, those registered for the Care to Chat will also have the opportunity to participate in at least one of four breakout sessions based on themes outlined earlier. We hope you can join us for what we believe should be an important and timely discussion on protecting the most vulnerable seniors against COVID-19.
END NOTES
[i] According to data provided by the BC Ministry of Health in July about twenty percent of cases of COVID-19 that resulted from outbreaks at B.C.’s long-term care homes were fatal, which is significantly higher than B.C.’s overall fatality rate of 6.1 per cent. See: COVID-19: Going Forward (BC Modeling update – July 20, 2020, accessed at:
https://news.gov.bc.ca/files/Covid19-Modelling_Update.pdf.
[ii] Canadian Institute for Health Information. Pandemic Experience in the Long-Term Care Sector How Does Canada Compare with Other Countries? June 2020. Accessed at: https://www.cihi.ca/sites/default/files/document/covid-19-rapid-response-long-term-care-snapshot-en.pdf
[iii] Public Health Agency of Canada. From risk to resilience: An equity approach to COVID-19. October 2020. Accessed at: https://www.canada.ca/en/public-health/corporate/publications/chief-public-health-officer-reports-state-public-health-canada/from-risk-resilience-equity-approach-covid-19.html#t2
[iv] Comas-Herrera A, Zalakaín J, Lemmon E, Henderson D, Litwin C, Hsu AT, Schmidt AE, Arling G and Fernández J-L (2020) Mortality associated with COVID-19 in care homes: international evidence. Article in LTCcovid.org, International Long-Term Care Policy Network, CPEC-LSE, 14 October. Accessed at: https://ltccovid.org/wp-content/uploads/2020/10/Mortality-associated-with-COVID-among-people-living-in-care-homes-14-October-2020-4.pdf
[v] According to Sept. 4th data from the Ministry of Health, since the first case of COVID-19 was reported in British Columbia in late January, 736 people have reported sick in health care settings (mostly in long-term care facilities), including 291 staff. One hundred and fifty-four people have died. In total, 211 people have died from COVID-19 related causes in B.C.
[vi] Covid-19 in Long-Term Care: Reflections from Ontario, Canada. Jour Nursing Home Res 2020;6:45-46. July 2020. Moser et al. Accessed at: https://www.jnursinghomeresearch.com/2301-covid-19-in-ltc-reflections-from-ontario-canada.html
[vii] Journal of American Geriatrics Society. Characteristics of U.S. Nursing Homes with COVID‐19 Cases. Hannah R. Abrams, Lacey Loomer, Ashvin Gandhi, and David C. Grabowski. June 2020. Accessed at: https://onlinelibrary.wiley.com/doi/full/10.1111/jgs.16661
[viii] Globe and Mail. Delays in COVID-19 testing results putting long-term care homes at greater risk. October 20, 2020. Accessed at: https://www.theglobeandmail.com/canada/article-delays-in-covid-19-testing-results-putting-long-term-care-homes-at/
[ix] Towards the end of October more than 100 seniors care residences in Canada were reporting outbreaks including 79 in Ontario, 14 in Alberta, 21 in British Columbia and 19 in Manitoba. (Source: Global News. Opposition, advocates say Ottawa needs to fix long-term care homes now. October 29, 2020. Accessed at: https://globalnews.ca/news/7431028/coronavirus-long-term-care-fixes/)
[x] Times Colonist. Long-term care deaths surged in COVID-19 first wave, Tam hopeful it won’t repeat. October 28, 2020 Accessed at: https://www.timescolonist.com/long-term-care-deaths-surged-in-covid-19-first-wave-tam-hopeful-it-won-t-repeat-1.24228755
[xi] BCCPA. BCCPA/EngAge BC release Pandemic “2nd Wave” Recommendations. July 28, 2020 Accessed at: https://bccare.ca/2020/07/bccpa-engage-bc-release-pandemic-2nd-wave-recommendations/
[xii] Eliminating staff ‘cross-traffic’ could have cut nursing home COVID-19 deaths by 44 percent, researchers find https://www.mcknights.com/news/researchers-find-how-44-percent-of-nursing-covid-19-deaths-could-be-prevented/
[xiii] SFU. GRC News covid-19 special issue risk, response, and resilience in an aging covid-19 world Summer 2020. Long-Term and Formal Community Care Gaps and Solutions. Article by D. Habib Choudhury. https://www.sfu.ca/content/dam/sfu/grc/stories/grc-news/GRC-News-Summer-2020.pdf
[xiv] American Health Care Association and National Centre for Assisted Living. REPORT: COVID-19 Cases in U.S. Nursing Homes. Updated October 19, 2020. Accessed at: https://www.ahcancal.org/News-and-Communications/Fact-Sheets/FactSheets/Report-Nursing-Homes-Cases-Oct19-2020.pdf
[xv] McKnight’s Long-Term Care News. COVID outbreaks tied to where nursing home staff live, researchers say. September 2020. Accessed at: https://www.mcknights.com/news/clinical-news/covid-outbreaks-tied-to-where-nursing-home-staff-lives-researchers-say/
[xvi] Journal of Post Acute and Long-Term Care Medicine. Evaluation of Testing Frequency and Sampling for Severe Acute Respiratory Syndrome Coronavirus 2 Surveillance Strategies in Long-Term Care Facilities. Charlotte Lanièce Delaunay, Sahar Saeed and Quoc Dinh Nguyen. August 2020. Accessed at: https://www.jamda.com/article/S1525-8610(20)30709-X/fulltext




