By Lara Croll
Concerns regarding the use of antipsychotic medications among residents in care homes have been well documented over the last two decades and are an ongoing concern.[i] The BC Office of the Seniors Advocate reports that 25% of residents in BC’s long term care homes are currently taking antipsychotics without a diagnosis of psychosis.[ii]
Antipsychotic medications, which were originally developed to treat people experiencing psychosis from illnesses such as schizophrenia, are often prescribed to manage the behavioural and psychological symptoms of dementia (BPSD). These behaviours, which can be complex and challenging for long term care staff to manage, can include agitation, anxiety, restlessness and even aggression.[iii]
While antipsychotic medications are often prescribed to manage these behaviours, they may provide limited benefit and cause serious harm, including increasing the risk of falls, infections, stroke, and even premature death.[iv] The Canadian Geriatric Society outlines that the use of antipsychotic medications should be limited to cases where non-pharmacologic measures have failed and where patients pose an imminent threat to themselves or others.[v]
In response to these concerns, numerous guidelines, resources and initiatives have emerged locally and across Canada to address the inappropriate use of antipsychotic medications among people with dementia. Examples of these initiatives include the Canadian Foundation for Health Care Improvement’s Antipsychotic Reduction Collaborative,[vi] and the BC Patient Safety and Quality Council’s Call for Less Antipsychotics in Long Term Care (Clear).[vii]
The BC Care Providers Association (BCCPA) also developed a member-led guide in 2013, which focused on successful interventions that safely reduced the use of antipsychotics medications in care homes. The guide, Best Practices Guide for Safely Reducing Anti-Psychotic Drug Use in Residential Care, remains one of the most accessed resources from the BCCPA’s website.[viii]
With these resources, care homes have made significant strides towards reducing the use of antipsychotics in care, down from 34% in 2012 to 26% as of 2016.[ix] However, despite significant awareness and efforts in this regard, the use of antipsychotic medications in BC’s care homes remains above the Canadian average (see Figure 1).
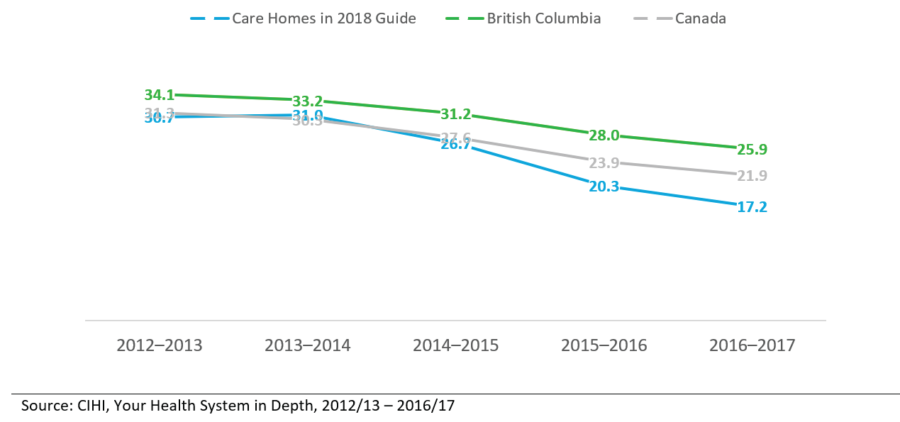
The widespread variation in the rate of antipsychotic use in care homes cannot be explained by resident characteristics alone. [x] Rather, it appears that the organizational culture of care homes, physician prescribing practices, and numerous other factors continue to play a determinative role.
Recognizing these ongoing challenges, the BCCPA’s Quality Committee has developed a renewed guide, entitled A Pathway to Ensuring the Appropriate Use of Antipsychotics in Continuing Care: Sharing Success Stories from BCCPA Members.
Structured around 11 profiles of BCCPA members, this guide provides real world examples of care homes that have successfully reduced their rate of inappropriate antipsychotic use through various non-pharmacological interventions. These profiles are presented in narrative form, allowing the reader to become fully engaged with successful approaches and to learn from challenges and lessons learned.
The purpose of this report is to share learning from a diverse group of care providers about how they developed a pathway to ensure the appropriate use these medications. The BCCPA believes that this guide will begin to bridge the knowledge and implementation gap and benefit future quality improvement work in our care homes.
The guide also identifies best practices and organizational change strategies that have led to cultural transformation and effective antipsychotic reductions (see Figure 2). Important principle include being person-centred and mindful of the risks and benefits of antipsychotic medications, working collaboratively within an interdisciplinary team, using validated tools and change management strategies, and fully involving the resident and their family in care planning are necessary both in the care home and community at large to reduce the use of inappropriate antipsychotic medications.
The BCCPA believes that the themes and best practices identified in the guide will not only assist care homes in providing the best quality, safety care for older person with dementia, but it will also highlight the structural challenges that the continuing care sector faces regarding this issue.
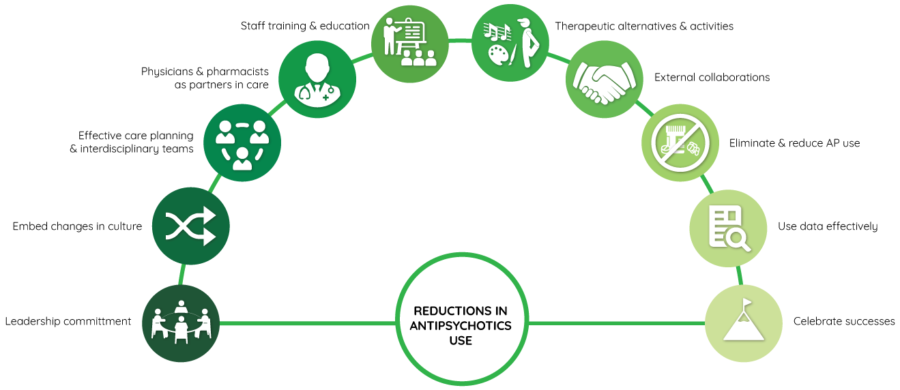
For example, one of the key strategies identified by the guide is the implementation of non-pharmacological management strategies for responsive behaviours in care homes. Care providers currently use many non-pharmacological approaches to manage behaviours, including music and art therapy, pet therapy, exercise programs, social engagement, and others. These programs are fundamental to the daily operation of a care home not only because they help manage complex behaviours but also because they provide meaning and quality of life to residents.
However, the fact that care providers continue to face challenges implementing these approaches in day to day practice highlights the complexity of caring for people with dementia in the current context. If funding and staffing challenges for nursing and recreation staff are not addressed, it is unlikely that the continuing care sector will be successful in its efforts to ensure the appropriate use of antipsychotics in the long term.
More broadly, the guide highlights the need for a societal shift in how our society approaches people with dementia. Traditionally viewed through a medical model of care, people living with dementia have been prescribed antipsychotics as a method to manage their behaviours – not just in long term care, but also in acute care and increasingly in the community. Shifting towards a psycho-social model of care that meets their needs, identifies what is important to them, and provides personalized care will require support and dedication at all levels of the health care system. As the number of seniors in our community grows, there is no better time for this shift than now.
END NOTES
[i] Crary, David. 2018. New report details misuse of antipsychotics in nursing homes. New York, 02 04. https://apnews.com/2052229826d84280aeb29208f7eb9434.
[ii] BC Office of the Seniors Advocate. 2018. Residential Care Quick Facts Directory, 2018 Summary. Vancouver: BC Office of the Seniors Advocate. https://www.seniorsadvocatebc.ca/residential-care-quick-facts-directory/.
[iii] Alzheimer Society of Canada. 2017. Understanding behaviour. Toronto, November 08. http://www.alzheimer.ca/en/Home/Living-with-dementia/Understanding-behaviour
[iv] Gupta, Sanjay, Prakash Masand, and Subramoniam Madhusoodanan. 2005. “Side effects of atypical antipsychotics in the geriatric population.” Current Psychosis & Therapeutics Reprots 3 (1): 26 -31. https://link.springer.com/article/10.1007/BF02629406.
[v] Choosing Wisely Canada, Canadian Geriatrics Society. 2014. Five Things Physicians and Patients Should Question. Toronto, April 2. https://choosingwiselycanada.org/geriatrics/
[vi] Canadian Foundation for Healthcare Improvement. 2018. Antipsychotic Reduction Collaborative – Reducing Antipsychotic Medication Use in Long Term Care. http://www.cfhi-fcass.ca/WhatWeDo/recent-programs/reducing-antipsychotic-medication-use-collaborative.
[vii] BC Patient Safety and Quality Council. 2018. Call for Less Antipsychotics in Long Term Care. Accessed January 15, 2018. https://bcpsqc.ca/clinical-improvement/clear/.
[viii] BC Care Providers Association. 2013. Best Practice Guide for Safely Reducing Anti-Psychotic Drug Use in Residential Care. Best Practice Guide, Vancouver: BC Care Providers Association. Accessed 11 16, 2017. https://bccare.ca/wp-content/uploads/Anti-Psychotics-Guide-hr-06-05-13.pdf
[ix] Canadian Institute for Health Information. 2018. Your Health System: In Depth. Accessed January 15, 2018. https://yourhealthsystem.cihi.ca/hsp/indepth?lang=en#/.
[x] Stokes, Julie A, David M Purdie, and Michael S Roberts. 2004. “Factors influencing PRN medication use in nursing homes.” Pharmacy World and Science 26 (3): 148 -154. https://link.springer.com/article/10.1023/B%3APHAR.0000026803.89436.a8.