By Rebecca Morris
In 2017 governments in both Ontario and British Columbia have made significant announcements directed at supporting the needs of seniors.
It will come as little surprise that provinces across the country are becoming attuned to the changing demographics which are expected to impact the delivery of health services in the coming decades. In fact, the portion of the Canadian population aged 65 and older is anticipated to rise by approximately 25% by 2036. Similarly, the number of seniors 80 and over is predicted to double between 2011 and 2036.
 In B.C. the proportion of the population aged 65 is anticipated to reach between 24 per cent and 27 per cent by 2038. Likewise, seniors in Ontario are expected to rise from comprising 15.2 per cent of the population to accounting for anywhere from 24 per cent to 26 per cent, within the same timeframe. Framed differently, by 2038 the mean ages in Ontario and B.C. are expected to be between 43 and 46 and 43 and 47, respectively.
In B.C. the proportion of the population aged 65 is anticipated to reach between 24 per cent and 27 per cent by 2038. Likewise, seniors in Ontario are expected to rise from comprising 15.2 per cent of the population to accounting for anywhere from 24 per cent to 26 per cent, within the same timeframe. Framed differently, by 2038 the mean ages in Ontario and B.C. are expected to be between 43 and 46 and 43 and 47, respectively.
So how are two populations with seemingly comparable demographics gearing up to meet the needs of seniors, both today and in the future and why does it matter?
In November, the Ontario government released Aging with Confidence: Ontario’s Action Plan for Seniors. The plan, which built on Ontario’s 2013 Action Plan for Seniors, is expected to result in $155-million being spent to improve seniors care over 3 years. In addition to these funds Ontario will spend $15 million over the next two years to upgrade “naturally occurring” retirement communities – i.e., apartment buildings which have high density of older adults.
The plan includes increasing the provincial direct care hour level to 4.0 hours of direct care, per resident, per day. Specifically, the government’s release states that:
Ontario will increase the provincial average to four hours of direct care per resident per day to ensure that residents in Ontario’s long-term care homes receive the highest quality of care. This will mean an additional 15 million hours of nursing, personal support and therapeutic care for long-term care residents across Ontario, and will ensure that every long-term care home in the province has staff with specialized training in behavioural supports and in palliative and end-of-life care. Four hours of care will mean increased flexibility around when residents can eat, dress or bathe, reductions in readmission to hospital for minor conditions that can be treated within the home, improved quality of work for staff, and reduction in inappropriate use of anti-psychotics, falls, restraint usage, pressure ulcers, pain and depression.
This announcement is timely, as Bill 33, the Time to Care Act, recently passed second reading . This private member bill, put forward by NDP Health Critic France Gélinas, would legislate a minimum care standard of 4.0 hours a day in Ontario’s long-term care homes.
The commitment to move toward an average of 4.0 DCHs was accompanied by the statement that 5,000 more long-term care beds would be developed over 4 years and that 30,000 much needed spaces would be developed over the next decade. Also included in the plan were significant investments in home care, including 2.6 million additional hours, over the coming year (which breaks down to 1.5 million hours for personal support services, 390,000 for nursing care, 110,000 for therapy, including physio & speech, and 600,000 for respite care), the development of an enhanced self-directed care model, and the announcement of a new provincial agency for home care.
To support independent, community dwelling seniors the province committed to a number of actions, which include: improving transportation options; making information easier to find through a one stop website; expanding the Age-Friendly Community Planning Grant Program; and strengthening elder abuse protections.
Further, Ontario has promised to invest $100 million over three years to support the 194,000 people in Ontario living with dementia. This will be done through Ontario’s dementia strategy (announced in April 2017) which aims to improve the lives of people living with the disease and their families. This includes an expansion of the Alzheimer Society of Ontario’s First Link program, through a 8.4 million commitment and investment of $37.5 million over three years to expand community dementia programs, including respite care services.
“This is the most significant commitment that the province has made in support of long-term care in over a generation. With more than 32,000 Ontario seniors on a waiting list for long-term care services today and the number set to rise, we need more system capacity,” says Candace Chartier, CEO, Ontario Long Term Care Association.
“In addition, ensuring that we are striving towards a publicly funded average of care hours across our homes will go a long way to enhancing the way we care for the most medically complex seniors.”
On the West Coast, the BC Ministry of Health released a new Action Plan to Strengthen Home and Community Care for Seniors in March. This coincided with a Ministry of Health announcement of $500 million in new funding for seniors care over four years as part of an Action Plan to improve care for seniors across the system, including increasing DCHs for seniors in residential care. Of  this amount, $275 million was intended to be provided over the next four years for home and community-care (HCC) services as part of the funding agreement with the federal government earlier this year.
this amount, $275 million was intended to be provided over the next four years for home and community-care (HCC) services as part of the funding agreement with the federal government earlier this year.
As outlined in the Government of British Columbia’s media release, annual funding increases over the next four years would enable health authorities to reach a consistent average of 3.36 DCH per resident day across both publicly https://bccare.ca/wp-content/uploads/2022/08/medcare-img22.jpgistered and contracted residential care homes. Prior to this announcement, attention to DCHs has also been noted as warranting attention by the BC Ombudsperson and the Office of the Seniors Advocate .
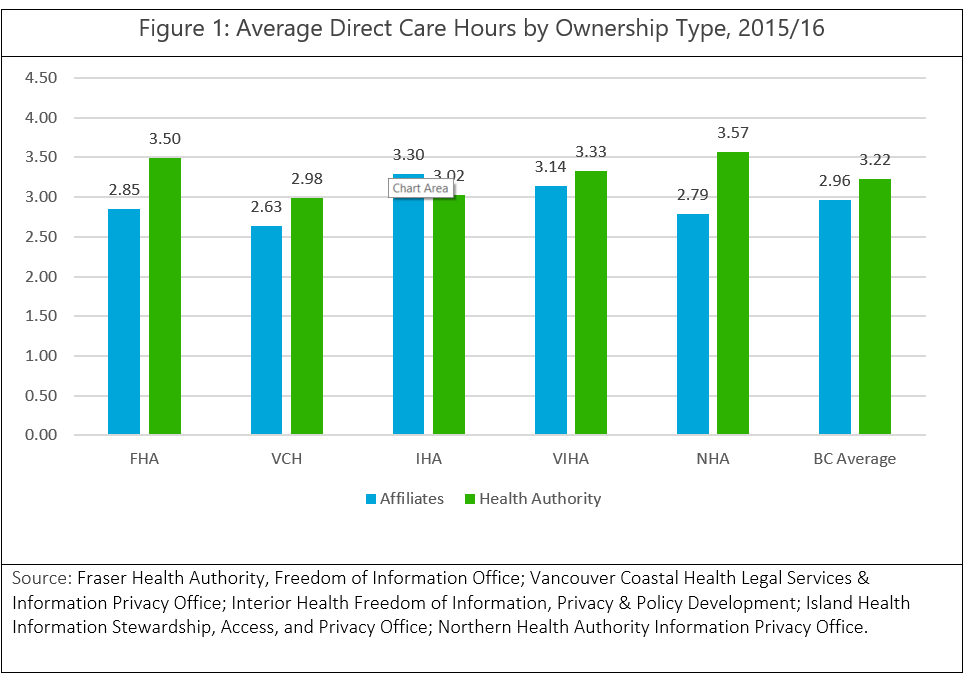 As noted in BCCPA’s “Care for the Facts” series, there are significant disparities in B.C. both between and within the Health Authority regions. These variations are particularly stark when care homes are broken down by ownership type. As demonstrated in Figure 1, in each health authority region, non-government care providers are funded for fewer DCH on average than government owned and operated care homes . This is further exacerbated by the fact the skill mix of staff included in a ‘direct care hour’ differs from health authority to health authority. With such disparities, it makes it difficult to provide equal and consistent levels of care, leaving some seniors at a disadvantage over others.
As noted in BCCPA’s “Care for the Facts” series, there are significant disparities in B.C. both between and within the Health Authority regions. These variations are particularly stark when care homes are broken down by ownership type. As demonstrated in Figure 1, in each health authority region, non-government care providers are funded for fewer DCH on average than government owned and operated care homes . This is further exacerbated by the fact the skill mix of staff included in a ‘direct care hour’ differs from health authority to health authority. With such disparities, it makes it difficult to provide equal and consistent levels of care, leaving some seniors at a disadvantage over others.
It should be noted that some research indicates that direct care staffing should be set at a minimum of 4.1 hours per resident each day – lending support to Ontario’s commitment to DCHs which are funded at 4.0 hours.
In addition to increasing funding for direct care hours, the BC Ministry of Health also committed to working with the Health Authorities to hire an additional 1,500 staff and announced of a $10 million grant, which has since been transferred to the BC Care Providers Association to manage a new province-wide Seniors Safety and Quality Improvement Program (SSQIP).
While the governments of B.C. and Ontario have both frequently noted a preference to support people at home, for as long as possible, no recent announcements have been made in terms of making funds available to increase the accessibility of home health services to British Columbians. Opportunities for supporting B.C. seniors to age in place include making resources available to increase minimum visit times, which are currently set at 15 minutes for congregate, or “cluster” care settings and 30 minutes for seniors residing in non-congregate settings and exploring the implementation of a “care-credit” model (or, as referred to in Ontario, a self-directed care model) in home health, to name just a few potential directions.
Ontario and B.C. are positioned to experience similar demographic shifts over the coming decades. Clearly, the actions which are taken now will affect the sustainability and efficacy of the continuing care sector.
Now, take a moment to think about how old you will be twenty-one years from now, or at very least how old your parents will be.
Put plainly, the investments made by our provincial governments today will impact what it means to grow old in each province in the future. Today, we are determining if tomorrow’s seniors will have the suitable workforce available to care for them; what the benchmarks will be for the quality of their care; and what choice seniors have in determining where, how and from whom they receive care.
Here’s to celebrating the 2017 successes for seniors care, and to ensuring that seniors care can continued to be strengthen as we head into 2018.
Footnotes
[i] Statistics Canada. Population Projections for Canada (2013 to 2063), Provinces and Territories (2013 to 2038).
[ii] Statistics Canada. Canada year book 2012, seniors
[iii] Statistics Canada. Population Projections for Canada (2013 to 2063), Provinces and Territories (2013 to 2038).
[iv] CUPE, Ontario. Major victory for Ontario’s Seniors: All party support for Bill 33 makes minimum care standards for seniors in long-term care closer to reality. November 2, 2017. http://www.marketwired.com/press-release/-2239404.htm.
[v] http://www.newswire.ca/news-releases/alzheimer-society-of-ontario-applauds-government-of-ontarios-investment-in-a-provincial-dementia-strategy-620665753.html
[vi] BC Ministry of Health. Significant funding boost to strengthen care for B.C. seniors. March 9, 2017. Accessed at: https://news.gov.bc.ca/releases/2017HLTH0052-000529
[vii] Ombudsperson. The Best of Care: Getting It Right for Seniors in British Columbia. Part 2. February 2012. Accessed at https://bcombudsperson.ca/documents/best-care-getting-it-right-seniors-british-columbia-part-2 .
[viii] Office of the seniors advocate. September 2017. Accessed at: https://www.seniorsadvocatebc.ca/app/uploads/sites/4/2017/09/Provincial-Results-Final-HQ.pdf.
[ix] BCCPA. Strengthening Seniors Care: A Made in BC Roadmap. January 2017. https://bccare.ca/wp-content/uploads/2017/01/BCCPA_Roadmap_ExecSummary_Jan2017.pdf
[x] CUPE back Gélinas bill to mandate at least 4 hours of care per long-term care resident. Nov 24, 2016. https://www.sudbury.com/local-news/cupe-back-gelinas-bill-to-mandate-at-least-4-hours-of-care-per-long-term-care-resident-472741