What follows is an opinion piece written by Michael Kary and published on our BCCPA website regarding the release of our policy paper.
+++
 When Canada’s Medicare system was created 50 years ago, the average life expectancy in Canada was 68.1 years. Today, the average life expectancy is 81.7 years, yet the health system has only marginally adapted to meet the needs of our aging population.[i] In particular, the health care system in Canada is still largely acute care oriented and not optimally designed to provide care for those with ongoing care needs, such as chronically ill elderly.[ii]
When Canada’s Medicare system was created 50 years ago, the average life expectancy in Canada was 68.1 years. Today, the average life expectancy is 81.7 years, yet the health system has only marginally adapted to meet the needs of our aging population.[i] In particular, the health care system in Canada is still largely acute care oriented and not optimally designed to provide care for those with ongoing care needs, such as chronically ill elderly.[ii]
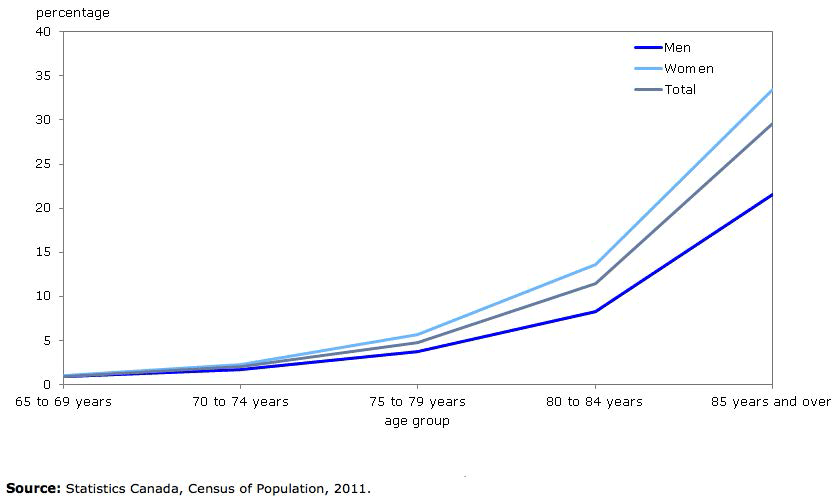
Currently seniors comprise about 14% of Canada’s population but account for almost half of health costs. By 2036, it is projected more than 25% of Canadians will be older than 65 and, by then, will account for 62% of this nation’s health costs.[iii] The number of seniors living in residential care will also increase as the proportion of seniors living in care homes increases with age. As Figure 1 below shows, only about 1% of people between the age of 65 and 69 live in residential care homes in Canada, yet nearly 30% of people aged 85 and older live in care-homes.[iv]
Figure 1: Percentage of Canadian seniors living in Residential Care (by Age Group)
Along with challenges with respect to costs and a health system that is not adequately designed to meet the needs of an aging population, there are also serious access issues. In 2012, for example, it was reported that 461,000 Canadians were not getting the home care they thought they required. Wait times for access to long-term care in Canada also ranged anywhere from 27 to 230 days.[v]
With the aging population and increased pressures facing the acute care system, now is the time to explore new solutions to meet these challenges and improve seniors care. Part of this will include redesigning the health system with new care models, but also targeted investments. A 2015 BC Care Providers Association (BCCPA) Commissioned Poll, conducted by Insights West, for example, indicates that the BC government should increase funding for long-term care. In particular, it found that:
- 62% believe that the health care system focuses too much on acute care and not on providing ongoing care needs, such as long term care or caring for the chronically ill elderly;
- 68% believe that the government does not provide adequate funding for residential care; and
- 84% believe that as seniors enter residential care homes with increased acuity or medical complexity, government funding should increase to meet these care needs. [vi]
In response to these challenges and the BC Ministry of Health’s current strategic priorities,[vii] the BCCPA has released a paper entitled Quality, Innovation, Collaboration: Strengthening Seniors Care Delivery in BC. As outlined in this new paper, the BCCPA advocates that the Health Authorities and Ministry of Health better utilize the existing capacity and expertise amongst non-government care operators, including developing strategies to reduce alternate level of care (ALC) beds and offset acute care pressures. As noted in the paper at a minimum such strategies should include the creation of a new publicly accessible online registry to report on ALC and vacant residential care beds as well as the use of current vacant beds within residential care homes, assisted living units and home support to reduce acute care pressures.
The BCCPA also recommends that these strategies be developed in the context of a new Continuing Care Collaborative comprised of government and non-government stakeholders, in order to foster open dialogue and a spirit of cooperation. Along with a new Collaborative, the paper also recommends that new designated funding be redirected to home and community care, including a minimum of 1% of acute care funding annually by the Health Authorities. As outlined in the paper, this funding could be allocated on annual basis over a five-year period into the continuing care sector.
This redirected existing funding would amount to approximately $320.8 million in the fifth year, which the BCCPA believes could go a long way to support the long-term sustainability of the sector and improve seniors care across the province. For example, based on initial cost estimates, $320.8 million directed to the continuing care sector could potentially fund the annual operation of 4,395 long term care beds;[viii] or 12,832,000 care aide hours;[ix] or 8,020,000 home support hours.[x]
Along with improving access, the new funding – in conjunction with the development of new continuing care models – will also help seniors to live in the most appropriate care setting. The BCCPA believes some of the acute care funding that is redirected to continuing care sector could be also be obtained through a reduction of ALC days. For example, assuming 50% of ALC days could be reduced by caring for patients in residential care homes instead of a hospital it could generate savings of over $200 million annually.
As outlined in the Quality, Innovation, Collaboration paper one of the focal points of redesigning the health system should be on the development of new continuing care hubs, which can provide enhanced care for seniors, including additional services such as dialysis, IV, sub-acute care, wound care, etc… The four key elements of the new continuing care hubs as outlined further in the paper include: 1) Integration of health professionals and family in seniors care; 2) New roles for care providers; 3) New funding models; and 4) Expanded role and co-location of services.
Finally, the paper in alignment with a recent report from the Seniors Advocate recommends that the province undertake a review of Assisted Living to remove the restrictions relating to the number of prescribed services (currently two) that may be provided in this care setting.
By undertaking the recommendations outlined in the paper the BCCPA believes it will help seniors access timely and appropriate care, reduce overall health system costs, and bring BritishColumbia to the forefront of innovation and sustainability in the continuing care sector.