This past week at BCCPA’s 2018 annual conference, three of B.C.’s foremost advocates for person-centred language in seniors’ care took the stage to talk about why “words matter”. The panel consisted of:
- Daniel Fontaine, CEO, BCCPA
- Maria Howard, CEO, Alzheimer Society of B.C.
- Jo-Ann Tait, Corporate Director for the Seniors Care and Palliative Services at Providence Health Care, as well as the Regional Program Director for Vancouver Coastal Health, serving Residential Care, Assisted Living and Supported Housing
The panelists sought to bring more intentionality to the words and phrases used in B.C.’s continuing care sector.
“Language affects how seniors and their families see themselves, how we do our work, the standards to which we aspire and even our own understanding of the work we do,” says Fontaine. “For these reasons we should be paying as much attention to language as anything else we focus on in the continuing care sector.”
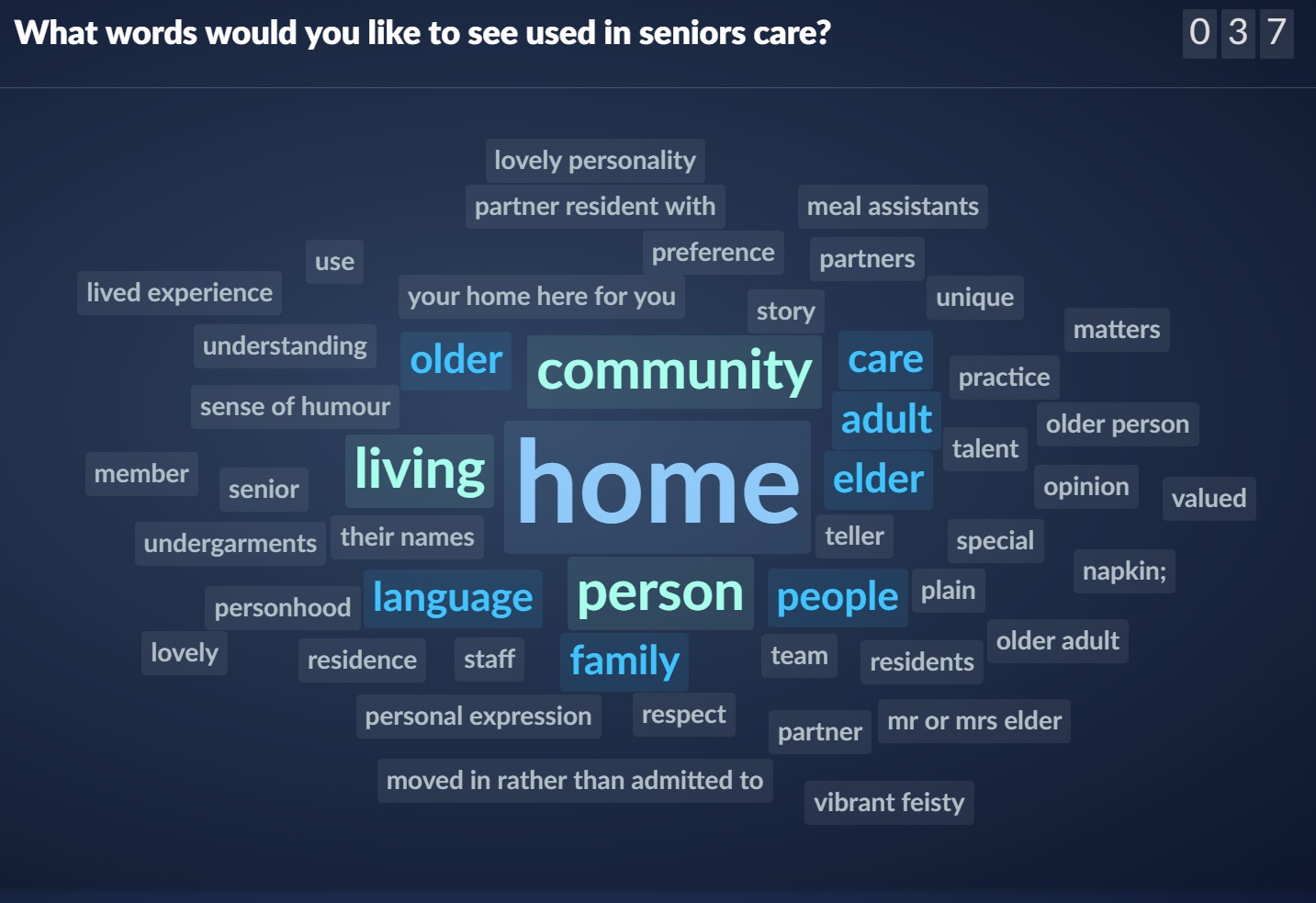
At the beginning of the presentation, participants were given the opportunity to contribute through an online tool in order to generate a web-based word cloud. Attendees were asked to submit which words or phrases they believe should be retired from the continuing care sector. Participants put forward words such as facility, demented, feeder, sweetie, senile, challenging, difficult, demented and violent. 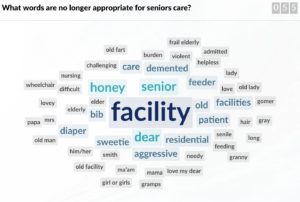
“I think that everyone in the sector would agree that exercises like these are important, but it is not enough to just develop a “do not use list”, we need to be in a constant state of reflecting on the attitudes and misperceptions behind the words we choose,” says Fontaine.
According to Tait, one way of doing this is using the “invisibility test”. This means asking oneself, does the language you are using make the person or their experience invisible. Beds, feeders or difficult, for example, would not pass this simple test.
Similarly, Howard reminded participants not to assume an experience for someone. Just because someone is diagnosed with dementia does not mean that they are necessarily suffering, nor does it mean that a caregiver is necessarily burdened. Instead, she suggests using terms like “living with dementia,” which are neutral and leave room for people to name their own experiences.
Drawing on her own experience in health care, Tait also discussed how using acronyms, over complicated language or jargon can be problematic. Tait advocated for doing-away with sentences filled with more letters than words and unnecessarily complex memos, and encouraged others to be clear, concise and to adopt the following mantra instead:
“Speak to your grandmother. If she can understand what you are saying, you’ve got it. Better still, if she can be in the room…Others will understand her.” 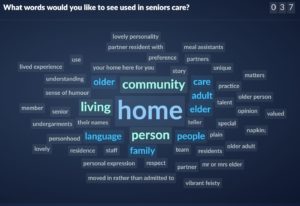
The panel ended with a participant-populated list of words which should be used in continuing care – they included, home, community, older adult, personhood, partners, preference and lived experience.
BCCPA has been consistently focusing on the importance of language over the last few years, including leading the call for the abandonment of the “F-Word” and we look forward to continuing an ongoing dialogue on this issue.